Healing the Cancer Divide by Expanding Clinical Trials
Innovation Reaching Colorado, the Rocky Mountain Region and Beyond
September 2022
What does health equity look like? For many people living in the U.S., access to high-quality care is out of reach. Everything from race, gender and ethnicity to income level or the zip code someone resides in can play a factor in equitable access to state-of-the-art care. Cancer adds another layer of complexity for those facing barriers to care, especially for minority populations in underserved urban and rural areas.
Cancer affects all population groups in the U.S. and is still the number one cause of death in Colorado. Yet for too long, medically underserved populations, such as rural or uninsured individuals, have been left behind by healthcare and are largely underrepresented in clinical trials. Investing in research that will lead to the cancer therapies of tomorrow is critical to understanding and reducing cancer disparities, and clinical trials are a key part of research that can lead to better treatments for people living with the disease.
We have patients from every county and corner of Colorado, so when we look at diversity, equity and inclusion, we want the population of clinical trial participants to represent more diverse groups. Everyone who walks through our doors has access to the highest quality cancer care because it’s the right thing to do. Full stop.”

Richard Schulick, MD, MBA
Director of the University of Colorado Cancer Center and Chair of the Department of Surgery, Aragón/Gonzalez-Guístí Endowed Chair in SurgeryAs a state and a nation, we must do more to address health disparities in the prevention, early detection and treatment of cancer among minorities in underserved populations. Enter the University of Colorado Cancer Center (CU Cancer Center), uniquely positioned to serve as a leader in the equitable healthcare space through partnerships with UCHealth University of Colorado Hospital (UCHealth) and the CU School of Medicine.
Raising the Bar on Cancer Care
In 1997, the CU Cancer Center was named a National Cancer Institute (NCI)-designated Comprehensive Cancer Center, an accomplishment shared with 52 cancer centers around the country at that time. The designation serves as a recognition of strength in advancing medical knowledge and clinical breakthroughs through scientific discovery, clinical trials and patient care. To this day, the CU Cancer Center is the only comprehensive cancer center headquartered in and serving the state of Colorado. It serves a massive geographic area with a much larger rural population than other centers across the U.S.



“There is a lot of privilege that comes with that designation but also a lot of responsibility,” said Schulick. “We have a nexus of world-class physicians and researchers discovering and delivering innovative cancer treatments right here on the CU Anschutz Medical Campus. We have a duty to exceed standards of care while also making cancer care equitable and diverse.”
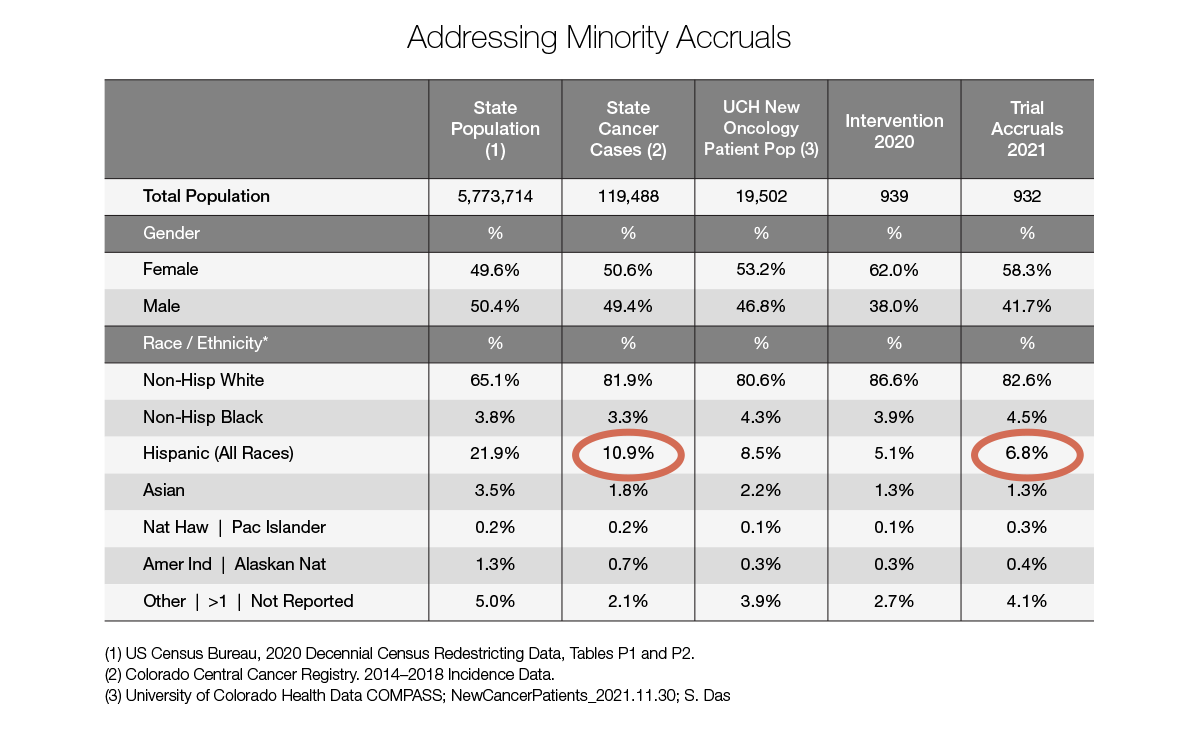
Through community outreach and engagement efforts focused on addressing disparities in care and outcomes particularly for Hispanic communities in Colorado, the CU Cancer Center hopes to increase the accrual of patients from Hispanic and rural/frontier communities in clinical trials as well as access to care for these populations at UCHealth.
“There has been a paradigm shift in healthcare over the last few years where we have gone from recognizing these disparities to actually doing something about it,” said Wells Messersmith, MD, FACP, FASCO, chief medical officer of oncology services at UCHealth, associate director for clinical services at the CU Cancer Center and head, division of medical oncology. “There are huge gaps in enrollment and clinical trial participation and various treatment options that are not going away with passive management. We need to address these disparities more quickly to provide equal care to all patients, regardless of race, ethnicity, gender or socioeconomic status.”
But success doesn’t happen overnight. Expanding the reach and access of clinical trials takes dedication and resources. Moving the needle more quickly requires the best physicians and investigators at the helm, backed by institutional partnership and support – and that’s where CU Anschutz shines.
In Good Company
In 2019, the Office of Community Outreach and Engagement (COE) was created within the CU Cancer Center to address barriers to cancer health equity and improve cancer outcomes in underserved areas of Colorado. With over 20 years’ experience addressing cancer disparities in prevention, control and survivorship, Evelinn Borrayo, PhD, professor and associate director of the Latino Research and Policy Center in the Colorado School of Public Health, CancerCure/AMC Cancer Fund Endowed Chair for Prevention and Control, was recruited as the CU Cancer Center's associate director for COE to spearhead these efforts.

Maps from the CU Cancer Center show that areas of Colorado’s Eastern Plains, Western Slope, and far south regions have rates of cancer frequency and outcomes like those in Appalachia. Alternatively, the Front Range and mountain communities along the I-70 corridor have cancer outcomes far better than national averages. Borrayo’s goal is to decrease cancer disparities and make sure that everyone in Colorado has equal access to cancer prevention, early detection and treatment.
“We’re trying to understand what kind of capacity exists to implement more evidence-based cancer interventions across Colorado regions,” Borrayo explained. “We tend to see a higher prevalence of cancer disparities in rural counties where there is a lack of knowledge and resources to tackle those disparities.”

Every five years, the CU Cancer Center is surveyed by the NCI to evaluate both successes and opportunities, certifying its place as a designated comprehensive cancer center. One of the areas of evaluation is how well the center collectively attracts and enrolls patients into clinical trials, highlighting the importance of the COE and collaboration across entities.
“The most recent NCI review in 2021 brought up an improvement opportunity to increase Hispanic and rural community representation to really bolster the community engagement piece,” said Borrayo. “We’ve made a concerted effort to bring all the [CU] parties together to find out how we can look at this more systematically.”
To do this, UCHealth and the CU Cancer Center created an Oncology Underrepresented Minority in Clinical Trials Taskforce chaired by Borrayo and several key players:



The taskforce is charged with tapping into the current 6.8% clinical trial participation rate among Hispanics to increase trial accruals and access of Hispanic patients to UCHealth, while also increasing engagement through collaborations with community-based hospitals like Denver Health that have a large percentage of Hispanic patients who don’t have access to clinical trials.
“We’re all very passionate about these inclusive engagement efforts because we know that patients do best when they’re on clinical trials and have access to life-saving therapies and treatments,” Lieu said. “We want to enroll patients that are representative of our state population, and we want the results that we see to be applicable to everyone. The only way to do that is to make sure we enroll a diverse patient population.”

This inter-entity leadership also allows the group to leverage its collective strengths and create a dialogue around needs and barriers across the organizations, further solidifying the invaluable relationship with campus hospital counterparts. “I think our hospital leadership realized that we need to go from a passive to an active role to provide equitable care across the state,” said Messersmith. “The fact that UCHealth is so closely aligned with the CU Cancer Center and the CU School of Medicine to give the best care possible to all citizens in Colorado is really special. We all want to do better.”
“I couldn’t ask for a better group of leaders to identify barriers, think through solutions, and drive implementation to support our patients and communities,” said Reed. “Oncology clinical trials represent the future of cancer practice and interventions for current and upcoming generations. To ensure these advancements are effective across patient populations, we must attract diverse cancer patients, provide excellent care and assess their interest in clinical trials.”
Breaking Barriers and Exposing Blind Spots
Getting to the root of the cancer disparity problem is an ongoing process. A lot of the work Borrayo’s team has done is centered around “the why” – why are people not accessing clinical trials? Is it us? Is it the community? Is there education that needs to be done? The answer to all these questions is a resounding “yes.”
As clinical investigators and as doctors, we need to be educated about our blind spots, for which there are many. For patients, I think there are misconceptions about clinical trials and a need for more education around the topic, and that means outreach to our community.”

Christopher Lieu, MD
Associate Director for Clinical Research at the CU Cancer Center and Co-Director for GI Medical Oncology, CU School of Medicine, Sohrab Amini, M.D., F.A.C.S., Endowed Chair in Pancreatic Cancer ResearchThe COE launched a Clinical Trials Education Program for anyone affected by cancer to help people better understand what it means to be part of a clinical trial. These 20- to 30-minute virtual education sessions are available in English and Spanish and help debunk some of the myths around clinical trials while covering general information on how to get enrolled. The COE also hosts various community events on policies and health fairs throughout the year to increase community engagement and build trust.
“I think it’s an awareness issue,” Borrayo said. “Most patients in general, but particularly from underserved communities, don't know what clinical trials are and whether or not they would even qualify. We want to show that there is a diversity of clinical trials; not all of them are treatment based and some of the prevention-type trials may be a better fit for some individuals.”
Other COE resources were developed to help increase the accrual of Hispanic subjects including developing a bilingual and bicultural clinical trials team and hiring a cultural and linguistic competency coordinator. Borrayo and Lieu also coordinate meetings with each of the disease-based teams at the CU Cancer Center and develop biannual reports on underrepresented minority accruals. By digging deeper into the data points on ethnicity, gender and age across disease types, they can identify trends of clinical trial participants and alert teams to potential red flags.

“Quite often the data will speak for itself when we look at the number of Hispanic patients, for example, that come through a particular clinic and how many actually enroll in clinical trials,” said Borrayo. “Compare those numbers to another ethnicity group like white, non-Hispanic, and the percentage of those clinical trial patients may be much higher at another clinic. We want to keep a pulse on this and provide feedback on how each disease-based team is doing to recruit more underrepresented minorities.”
Although there are some misconceptions around clinical trials, access hurdles are what make it difficult for cancer patients to fully participate in the process. It takes a village to conduct a clinical trial, and there is often a burden placed on the patient to navigate extra visits and procedures while they may already be driving long distances to come to the CU Cancer Center and addressing concerns about paying for extra costs. The COE is investigating ways to make transportation and housing more affordable.
“It’s not just about offering a clinical trial,” Lieu said. “It’s also about making it as feasible as possible for people. There are a lot of other factors at play like ‘who’s going to drive me to my appointment?’ or ‘who’s going to watch my kids while I have to stay overnight?’ We need to think holistically about the patient experience and even the playing field as much as possible.”
The Transformative Power of Giving
In the realm of what’s possible for equitable healthcare, the alignment between COE, the CU Cancer Center and UCHealth is what makes CU Anschutz stand out among academic medical centers. This should be the model of what cancer care can look, feel and be like. And it’s only the beginning.
“It’s an honor to work with people like Dr. Borrayo and Dr. Lieu because of the depth and breadth of experience they bring to the table,” said Reed. “If we attract great people and prioritize the work at COE, we will continue to contribute great science and clinical care to society.”
The best way to move the needle to affect real change is by attracting and retaining top talent like Borrayo, who now holds an endowed chair thanks to philanthropic support. The CancerCure/AMC Cancer Fund Endowed Chair for Cancer Prevention and Control provides protected time for Borrayo and her team to focus on this important work. Both groups have a long history of supporting the innovative research taking place at the CU Cancer Center; in 2005, the AMC Cancer Fund became affiliated with the CU Cancer Center with a focus on raising awareness and funds for the CU Cancer Center's programs in prevention, care, education, research and service to the nation. CancerCure first started supporting the CU Cancer Center in 1997 when people traveled from all over the Rocky Mountain region for cancer treatment.
"In 2017, we partnered with the Anschutz Medical Campus to create the Cancer Prevention and Control Endowed Chair to support Dr. Borrayo and her team. Knowing these funds are going toward attracting top talent like Dr. Borrayo is very gratifying. Her goal to decrease cancer disparities and make sure everyone in Colorado has equal access to cancer prevention and treatment is the direction we want our philanthropy to support.”
CancerCure Co-Chairs:
Midge Wallace, Carolyn Fancher and Nina AhbeThe work of COE, the CU Cancer Center and UCHealth is vital, and we intend to keep pushing this forward to ensure underserved communities aren’t left behind. It is through philanthropic support and cross-campus partnerships like this one that the CU Cancer Center’s vision becomes reality.

Laura Strand
CU Anschutz Fund for Excellence
To provide a flexible funding source to address CU Anschutz's most promising priorities in support of research, education and patient care.